© Constance J. Moore
Colonel, ANC (Retired), ANCA Historian
During World War I, experienced Army nurses and attendants were embedded in all major hospital centers in France to provide definitive care to the psychologically injured. Nurses established trusting relationships with these traumatized soldiers in order to calm their fears.1
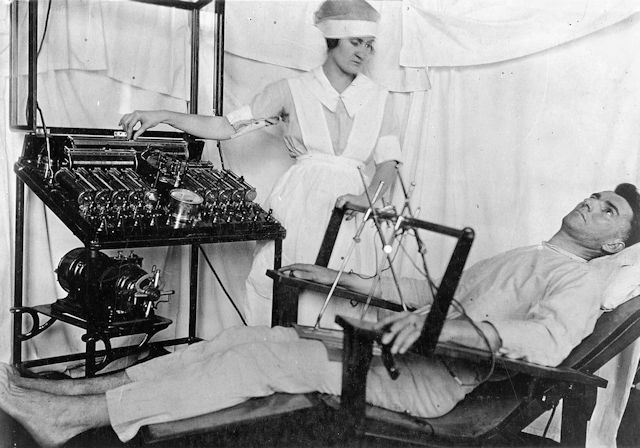
Patient receiving Faradic (electroshock) treatment |
Patients were observed and assessed for return to duty. Those deemed to have major psychiatric disorders, which rendered them “insane” or incompetent, were then transferred by train to Base Hospital No. 116, where they were stabilized for transport to the United States. In this pre-antipsychotic medication era, many patients were quieted, and comforted by the hydrotherapy, and the rudimentary faradic (electroshock) therapy, as they were prepared for their journeys home.
2
When they were calmed and cooperative, the psychiatricaly ill were transferred as a group to Army psychiatric hospitals in the United States with their own escorts. They were well managed by their support staff. The Army reported that no patients in this classification group required restraints or committed grievous bodily harm to themselves or others during their long sea journeys.3
Patients who were diagnosed with “shell-shock” or transient stress-induced psychological disorders, were moved to Base Hospital No. 117. This facility was established twenty-five miles from the front because the Army adapted a strategy discovered by the English and the French. They found a high rate of recovery when stress-related casualties were treated closer to their units.4
Nurses were considered key to the recovery of these individuals. Their major function was managing the ward environment. “The social atmosphere of the ward was all important. An atmosphere of cure was necessary in order to successfully cope with the patient’s mental attitude.”5 Nurses encouraged patients to take responsibility for their own actions so they would develop confidence for recovery.
Nurses created detailed ward routines that kept patients busy from early morning until late at night. For example, all patients were awakened and standing at their bed side for inspection at 4:00 a.m. No one was allowed to remain in bed unless he was ill. After breakfast and ward rounds with the psychiatrist and head nurse, patients exercised, and were required to train on machine guns and grenades.
Next on the schedule the patients were quickly ushered to various work details. The duty roster included assignments like road work, yard manicuring, cleaning kitchens, and washing ward linen. Patients also could take courses “in bench woodwork, carpentry, painting and staining, machine work, pattern making, automobile mechanics, English, arithmetic, bookkeeping, stenography, typewriting, drafting and designing, geography, agriculture, history, economics, weaving, basketry, printing, lettering, and poster making.... [Additionally,] entertainments of various kinds were given, with an effort to have the patients put on their own shows, and a band was organized.”6
During these daily activities, the staff observed how the patients multi-tasked, sequenced tasks, and got along with their peers. Nurses and other staff members could determine if their patients’ judgment improved, their strength returned, and they demonstrated hardiness. The whole idea was for patients to recover from the serious stress reactions through rapid engagement and hope for returning to duty.
Nurses worked with patients in the evening and throughout the night time and watched their interactions with other patients. They were aware if the depressed or moody patients were sad and kept to themselves or engaged with others. Nurses saw how the highly emotional, dramatic, and hypo-manic individuals either could calm themselves or required thoughtful interventions by the staff. This information was important to the assessment for patients’ readiness to duty.
As one doctor stated “It is the nurse who must lead the patients, individual by individual, back to health.... Find the rate of recovery in any particular hospital for this type and I can tell you pretty much what kind of a nursing corps there is in that hospital.”7
1 Thomas Salmon and Norman Fenton, eds., The Medical Department of the United States Army in the World War, vol X, Neuropsychiatry (Washington, DC: U.S. Government Printing Office, 1929), 281.
2 Ibid., 129.
3 Ibid., 284.
4 Lorraine Davis, Sen. Ed., War Psychiatry (Washington, DC: Office of the Surgeon General, 1995), 9.
5 Thomas Salmon and Norman Fenton, eds., The Medical Department of the United States Army in the World War, vol X, Neuropsychiatry (Washington, DC: U.S. Government Printing Office, 1929), 360.
6 Thomas Salmon and Norman Fenton, eds., The Medical Department of the United States Army in the World War, vol. X, Neuropsychiatry (Washington, DC: U.S. Government Printing Office, 1929), 278, 96.
7 R.E. Williams, “Organization and Scope of Neuro-psychiatric Unit,” American Journal of Nursing 18, no. 11 (August 1918), 1020.